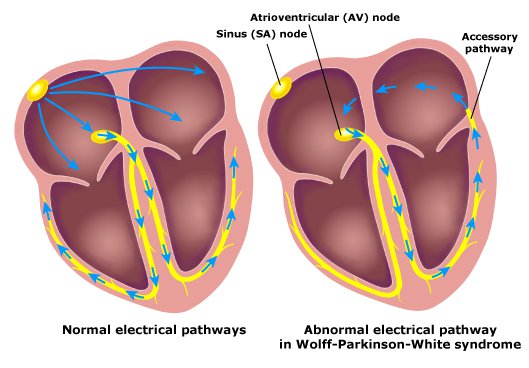
In Wolff Parkinson White Syndrome or WPWS in short, an additional electrical pathway developed between the upper and lower chambers of the human heart triggers a rapid heartbeat. It is worthwhile to note that this condition is congenital and fairly rare.
The episodes of rapid heartbeats generally are not regarded as life-threatening. Nonetheless, serious heart issues can develop. Timely treatment can prevent or stop such incidences. A catheter-guided ablation procedure can permanently fix the problems related to one’s heart rhythm.
A vast majority of people having an additional electrical pathway do not experience fast heartbeat at all. This condition, known as the Wolff-Parkinson-White or WPW pattern, is discovered by chance only at the time of a heart examination. While the WPW pattern is deemed harmless most of the time, healthcare professionals might suggest further evaluation in kids with WPW pattern, before they are allowed to take part in physically demanding sports.
Causes of Wolff Parkinson White Syndrome
The human heart is made of one pair of upper and lower chambers, each, which are known as the left and right atrium and the left and right ventricle respectively. The sophisticated bioelectrical circuitry of the heart signals it when to contract and if an additional electrical connection is present inside this vital organ, the entire circuit is shorted, causing the heart to beat irregularly or even too fast.
In any WPWS patient, the atria and the ventricle cannot communicate properly, and the electrical impulses traverse the normal electrical node of that person’s heart, making the ventricle to contract earlier than it should. WPWS affects one to three in every thousand people.
It is still an unsolved medical mystery what makes this additional electrical pathway to form. However, it is observed that a small number of persons suffering from WPWS carry mutated genes, and others are found to be born with heart defects. In WPWS infants, about two in every ten are diagnosed with Ebstein’s anomaly, which can be attributed to the abnormalities of the tricuspid valve located on the right part of the heart.
Symptoms
People corresponding to all age groups, including the infants, can experience WPWS symptoms. Symptoms of WPWS are the outcome of a quickly beating heart, and they usually make a maiden appearance in individuals in their twenties or teens.
Non-severe symptoms
- Experiencing pounding, fluttering, or rapid heartbeats
- Breathing issues (shortness)
- Lightheadedness or dizziness
- Fatigue
- Fainting
- Anxiety
An incidence of a very rapidly beating heart can begin all of a sudden and could last for as little as few seconds or as much as several hours. Such episodes can happen while at rest or at the time of exercise, and alcohol and any other stimulants including caffeine may act as a trigger for a number of people.
Over time, WPWS symptoms may cease to exist in up to one-fourth of people who had had the syndrome.
More critical symptoms
About one to three in every ten individuals diagnosed with WPWS occasionally experience a kind of irregular heartbeat, i.e., atrial fibrillation; and the following symptoms and signs may occur in such a group of people.
- Chest tightness
- Chest pain
- Fainting
- Difficulty breathing
Symptoms (infants)
- Ashen color
- Rapid breathing
- Irritability or restlessness
- Poor eating
Diagnosis
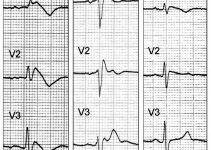
- Electrocardiogram or ECG: Tiny sensors attached on the patient’s arms and chest record the electrical signals that travels through that person’s heart. The medical practitioner looks for patterns that suggest that an additional electrical pathway is present in the heart of the person subjected to an ECG.
- Portable ECG or pECG: The whole procedure is arranged at home, and the Holter monitor registers the activities of the patient’s heart for twenty-four hours. When the subject is experiencing a rapid increase in heart rate, an event monitor records that activity.
- Electrophysiological testing or EPT: Catheters armed with electrodes are made to pass through the blood vessels up to several areas in the patient’s heart. The electrodes can specifically map how the electrical impulses are spreading at the time of every heartbeat, and also identify the existence of any additional electrical pathway.
Differential Diagnosis
Diagnosis of hypertrophy, myocardial infarction or MI, and bundle branch block or BBB in instances of WPW syndrome are all obscured.
- Type A WPWS should be distinguishable from the following heart-related conditions
- Right ventricular hypertrophy or RVH
- Right BBB or RBBB
- Inferior MI
- True posterior MI
- Type B WPWS should be distinguishable from the following heart-related conditions
- Left BBB or LBBB
- Inferior MI
- Anterior MI
- WPW syndrome and atrial flutter
- Paroxysmal VT (ventricular tachycardia) or flutter
Treatments
The treatment is decided by various factors, including the frequency and the severity of the symptoms. If the patient does have the WPW pathway, but not any symptoms, then that person is unlikely to receive any surgical procedures or scheduled medication. In case treatment is required, the objective is to slow down a fast heart as soon as it happens and to prevent any such episodes in future.
The specialist may suggest from the following option for treating WPWS.
- Vagal maneuvers: These simple movements of the human body; such as bearing down in the way one has a bowel movement, coughing, and applying a pack of ice on the face; they all affect vagus nerve that helps to regulate the heartbeat.
- Medications: If the vagal movements do not prove to be beneficial in one’s case, then the doctor may consider injecting the patient with an anti-arrhythmic drug.
- Cardioversion: When the first two alternatives prove to be ineffective; the physician may use patches or paddles on the patient’s chest to send a train of electrical impulses to shock the heart, which in turn, helps to restore the normal rhythm.
- Radiofrequency catheter ablation or RCA: It is considered the last line of treatment for WPWS, where catheters are passed through the blood vessels of the patient’s heart. The electrodes fitted at the tip of a thin, flexible tube are heated to melt and dissolve the additional electrical pathway in question permanently.
Prevention
Though it is not possible to prevent the occurrence of WPWS, a large number of people are typically found to be receptive to appropriate therapies, as prescribed by the consultant electrophysiologist or the consultant cardiologist.
Prognosis
The prognosis for this syndrome is excellent. In general, many individuals diagnosed with WPWS may never require any treatment.
When to visit a doctor?
Many medical conditions can trigger arrhythmia, i.e., irregular heartbeat. It is crucial to seek a prompt and accurate diagnosis and appropriate care. Call the doctor immediately if one or some of the following symptoms last beyond a few minutes.
- Irregular or rapid heartbeat
- Chest pain
- Difficulty breathing