Tay Sachs disease Information
Tay-Sachs disease is a condition that mostly affects children wherein the genetic lipid storage is affected with fatty substances such as ganglioside. This fatal disease is also called as GM2 gangliodosis or Hexominidase A deficiency is and named after the physician who first saw the red spots in the retina which is a symptom of this disease. His name is Warren Tay, an ophthalmologist.
What is Tay Sachs Disease and How It Affects the Child
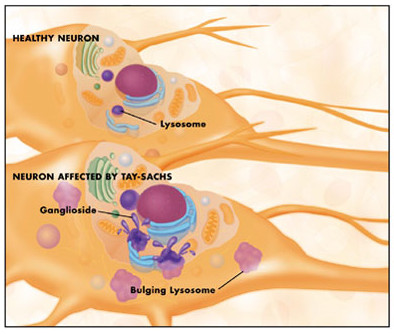
Basically, this disease is a genetic problem wherein a defective gene is copied by the child from the parent’s DNA. Usually, the child with this problem appears to be developing normally in the first few months but after about 6 months, it gets worst. The because of the gangliosides accumulating in the nerve cells of the brain, the nerve cells become distended with fatty materials. The child then develops to be blind, deaf, or having dysphagia.
In some cases, where it is rare, it affects patients in their twenties or thirties. During this stage, the patient develops to have neurological problems and they have unsteady gait.
Tay-Sachs disease affects the Jews mostly. It affects about one in every twenty of Ashkanezi Jeweish decents and death occurs one in 360, 00 0 newborns worldwide.
Types of Tay Sachs disease
- TYPE 1 GM2 gangliosidosis which is known as the classic infantile Tay-Sachs disease
- TYPE e TIII GM2 also known as the juvenile sub acute TSD
- THE B1 variant of GM2 gangliosidosis which is a late infantile acute to chronic Tay-Sachs disease
- GM2 gangliodosis which is the chronic type of Tay-Sachs disease
Tay Sachs disease Causes
The absence of a gene that is called HEX A is what causes the Tay-Sachs disease. When a person has no HEX A gene, there is an absence of metabolic pathway which is necessary to avoid the deposition of fats in the nerve cells.
Tay Sachs disease Symptoms and Signs
The symptoms for Tay Sachs disease will not appear until the child is at 3 to 6 months. In acute phases, this includes:
- Seizures
- Decreased eye contact
- Listlessness
- Increased irritability
- Delayed mental and social skills
- Slow body growth but the head size is increased.
- Changing behaviors such as the infant doesn’t smile, crawl, or doesn’t roll over
When the problem progresses, these are the signs and symptoms
- Abnormal body tone
- Deafness
- Loss of intellectual skills
- Loss of motor skills
- Feeding problems
Tay Sachs disease Pictures
 Picture 1 : Tay-sachs disease – healthy neuron and neuron affected by Tay-Sachs
Picture 1 : Tay-sachs disease – healthy neuron and neuron affected by Tay-Sachs
Image source: sfn.org
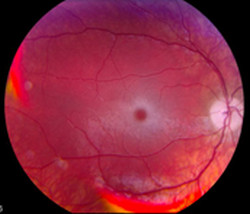
 Picture 2 : Photograph of Fundus showing changes in the retina and is associated with GM2 gangliosidosis
Picture 2 : Photograph of Fundus showing changes in the retina and is associated with GM2 gangliosidosis
Image source : wikipedia.org
 Picture 3 : Tay-sachs Chromosome
Picture 3 : Tay-sachs Chromosome
Image source : ncbi.nlm.nih.gov
Tay-Sachs disease Diagnosis
In diagnosing a Tay-Sachs disease, physical examination is done where the ophthalmologist will examine the eyes of the patient wherein “cherry-red” spot is seen at the back of the eyes. Detailed family history and hereditary disorders are also checked by the physicians.
Aside from that, blood tests are taken to measure the HEX a or hexosaminidase A activity. This is the main indicator if the child has the disease.
Tay-Sachs disease Treatment
Unfortunately, there are no treatments for Tay-Sachs disease. Anticonvulsants are given to control seizure. Supportive or Palliative treatments are also given especially in nutrition and hydration and ways to keep the airway open. Feeding tubes are attached to children since motor skills are affected.
Tay-Sachs disease Prevention
There are multiple ways on assessing the possibility of having a Tay-Sachs disease
Screening
- Carrier testing- this is usually done by couple who are at risk for acquiring this problem. This test aims to detect if an individual is carrying the copy of the genetic mutation.
- Prenatal testing– this test is done to know if the fetus has inherited the defective genes from each parents.
Enzyme Essay Techniques – the test determines if the person has low HEX A.
Mutation Analysis Techniques – this technique is done where tissue samples are obtained by using minimal invasive techniques. This technique screens many mutations however it can leave a small possibility of both false positive and false negative results. Nonetheless, it can still help in predicting the condition.
